We have interviewed Dr. Raúl Córdoba, MD, PhD. Head of the Lymphoma Unit at the Fundacion Jimenez Diaz University Hospital, Madrid, Spain. Chair of the EHA Scientific Working Group.
- Much progress has been made in cancer treatments, but the quality of life of patients is still a pending task. What consequences or side effects can cancer patients experience?
Thanks to the advances we have made, especially in the last decade, in new treatment options for cancer patients, we have managed to increase survival in many types of cancer, and we have increased the percentage of cured patients. We call “long cancer survivors” those people who are more than 5 years free of disease and treatment. In pathologies such as some types of lymphomas, a hematological cancer that affects the lymphatic system, cures exceed 90%. This means that patients are cured of their cancer, but live in the long term with the sequelae of the treatments that we have had to administer to achieve their cure, which can significantly affect their quality of life.
- The RESILIENCE project seeks precisely to improve the quality of life of cancer patients after treatment with anthracyclines, but what is its importance?
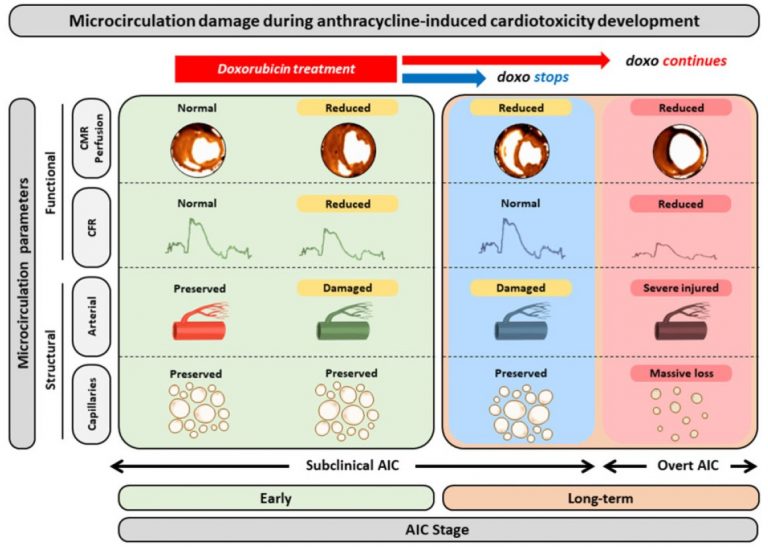
One of the problems that patients may face, both during treatment and in the medium and long term, are heart and cardiovascular diseases. Anthracyclines are a group of highly effective anti-tumor drugs that are widely used in some types of tumors, such as lymphomas, leukemias, breast cancer and sarcomas, among others. When we have a highly effective treatment, which achieves excellent results in both cancer control and cure, we must weigh the expected risks and benefits of such treatment in each of our patients. If the balance tips in favor of the benefits of cardiotoxic treatment, we must take extreme measures to protect the heart.
- Why have patients with Non-Hodgkin’s Lymphoma been selected as the target population for this clinical trial? Will it be extrapolated in the future to patients with other types of cancer?
Not all tumor types that can be treated with anthracyclines receive the same doses. We know that the cardiovascular toxicity of anthracyclines is “dose-dependent”, i.e., the higher the dose, the greater the risk of toxicity to the heart. Non-Hodgkin’s lymphomas will always exceed this maximum dose threshold, so precautions must be taken in all patients. Regarding the extrapolation of the results to other patients with other types of cancer, everything will depend on the planned dose of anthracyclines in their treatment schedules.
- Clinical trials can sometimes generate reluctance among patients. How do they react when you talk to them about RESILIENCE?
In the field of hematology and oncology, patients are very well informed, both by their medical teams and by patient associations. There is still a lot of ignorance about what clinical trials are, but many patients are already asking directly about them, to see if there are any treatment options different from the conventional ones, and with a better tolerability profile. In this regard, when we explain to them the risk of toxicity to the heart for the treatment that we consider to be the most appropriate for treating their case, and that we have a possibility of taking better care of their heart both in the short and long term, it is a proposal that almost all patients usually accept. We are offering them care to protect their health in the long term, which makes them think that we are thinking beyond the months of chemotherapy.
- The name of this project invites us to think about resilience. How would you define it and why is it so important?
Resilience is the ability to adapt to a new event. In the case of cancer, patients have to adapt to a new situation, and receive treatments that, although the aim is to control or cure the cancer, can produce side effects that are sometimes serious. Preparing the body to receive these treatments and to better adapt to the external changes that we are going to provoke, means that tolerance to the treatments is better and allows us to meet the treatment objectives and not have to delay treatments, reduce drug doses or even suspend them, which could compromise the prognosis of the patients.
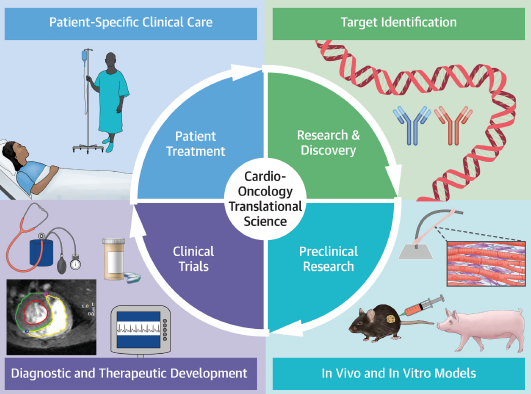
- You have participated in the recent clinical practice guidelines of the European Society of Cardiology related to cardio-oncology. How do you assess this integrated management of cancer patients? How do you think patients benefit from this multidisciplinary approach?
We cannot continue to do medicine as we did 10-20 years ago. Things have changed a lot in the last few decades. A single physician cannot control all aspects of a patient’s health. We physicians have to be aware that we are part of a team in which each one brings the best of himself, his knowledge and his experience. Hence, present-day medicine is geared towards teamwork and a multidisciplinary approach to patients. In the case of cancer patients, and in my case, lymphoma patients, a hematologist like myself must ensure that the patient receives the most individualized treatment possible. This is not possible without the close collaboration of other specialists such as radiation oncologists, nurses, hospital pharmacists, geriatricians, psycho-oncologists, and a host of other professionals who support us in providing the best possible care for our patients. And in recent years, cardiologists have joined this team, training and specializing in the discipline of Cardio-Oncology. In this respect, the European Society of Cardiology guidelines on Cardio-Oncology are the manifesto of this teamwork, in which each author and each scientific society that has collaborated (I have acted as representative of the European Association of Hematology) has contributed its knowledge to make recommendations that can be followed by all professionals who treat cancer patients, wherever they are in the world. The recommendation guidelines are simply a way of “democratizing” and making expert knowledge more accessible to the entire medical community.